Around 15-20% of the adult population experience infertility, due in part to the trend to delay starting a family, but also due to adverse conditions in environment and lifestyle.
In couples experiencing infertility, male and female infertility account for around 30% each, with a further 30% due to combined male/female causes, and the remaining 10% unexplained.
Female Infertility
Approximately 20% of female infertility is due to blockage of the fallopian tubes; small, delicate organs that capture the egg released during ovulation and transport it towards the uterus where it is fertilized to become an embryo that then implants in the lining of the uterus. Blockage of the fallopian tubes often results from scarring due to surgery and/or infections, like Pelvic Inflammatory https://www.doctornaumann.info/tadalafil-equivalente/ Disease or Chlamydia. The remaining 80% of female infertility is caused by a variety of factors that may include:
Male Infertility
Male infertility is an increasing problem around the world, often resulting from lifestyle and environmental factors. Other causes may include varicocele (enlargement of veins in the scrotum, like varicose veins), dove acquistare levitra infection, and unsuccessful reversal of vasectomy. In men, hormonal deficiencies are quite rare but can cause insufficient sperm production.
Measuring Fertility Potential
Empirical data show that female fertility declines significantly after the age of 35 years. Although individual differences do permit some women in their 40s to conceive, generally speaking egg production progressively declines.
There are tests that measure the potential of the ovaries to produce eggs. These include Antral Follicle Count (AFC) of the ovaries by transvaginal ultrasound and a blood test for the Anti-Müllerian Hormone (AMH).
Infertility Investigations
Couples seeking assistance to have a child should expect to undergo the following investigations, some mandatory and others appropriate to individual circumstances:
Assisted Reproduction Techniques (ART)
Cycle Monitoring is achieved by a combination of ultrasound scanning and hormone assays from blood samples. This allows the development and maturation of eggs to be monitored.
Ovarian Stimulation is achieved by the administration of hormones in combination with cycle monitoring and can be used in both Intrauterine Insemination (IUI) and IVF treatment.
Oocyte (egg) Collection is performed via the vagina under anesthesia, for use in conventional IVF or ICSI.
Conventional IVF is the combining of eggs and sperm in a test tube to allow spontaneous fertilization and the early development of an embryo.
ICSI involves injecting sperm into an egg to achieve fertilization. This technique can be used to overcome most forms of male infertility.




 ICSI sequence
ICSI sequence
PESA and TESA are procedures to obtain sperm either from the testicle itself or from the epididymus (sperm storage organ). These procedures can be used to locate sperm where none is found in the ejaculate.
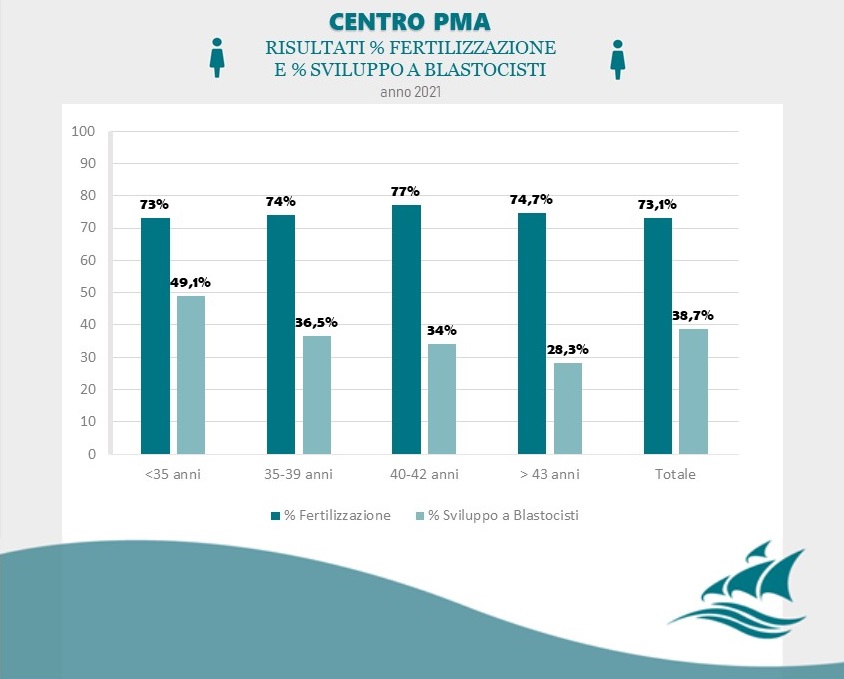
When the fertilized egg/embryo has developed for 5 days it is called a blastocyst. At this stage it has shown resilience and has an estimated implantation rate of over 60%.
At the blastocyst stage, a biopsy allows investigation of chromosomes and genes. These techniques are aimed at preventing the transfer of pathological embryos and avoiding invasive tests in later pregnancy, like amniocentesis.
Pre-Implantation Genetic Screening (PGS) provides information about trisomy as in Down Syndrome, or absent chromosomes.
Pre-Implantation Genetic Diagnosis (PGD) provides information about single genes like that responsible for cystic fibrosis.
Assisted Hatching is a technique that facilitates the development of the embryo and improves the process of implantation. In some cases the protective shell (zona pellucida) covering the early embryo fails to dissolve, meaning that the embryo cannot ‘hatch’ and develop to a stage where it is capable of implanting in the lining of the uterus. In assisted hatching, the dissolution of the zona pellucida is assisted by the application of a special solution or laser.
Embryo Transfer is performed by using a smooth and fine catheter. The procedure is not painful and does not require anesthesia. The placenta develops around two weeks later when the embryo starts implanting into the lining.
Cryopreservation (freezing) is offered for embryos not used for transfer. Freezing allows their use even years later with the same pregnancy rates as for freshly transferred embryos.
Social Freezing
Social Freezing is freezing of eggs for non-medical reasons, like the personal preference of postponing pregnancy, which can bring with it concerns about diminishing or lost fertility with increasing age, especially for women aged from 35 onwards. In effect, freezing eggs conserves a woman’s fertility for future attempts at pregnancy.
Oocyte Donation
is the only ART option for women who are not able to produce their own eggs due to diminished ovarian function or the onset of early menopause. The donor undergoes ovarian stimulation to produce eggs that can be collected and used in IVF with the sperm of the male of the recipient couple. Only women under the age of 35 who have already had children are suitable to donate eggs resulting in a conception rate of slightly over 50%. Donors are comprehensively screened and matched with a recipient couple, for things like physical characteristics and blood type.
To know more about Oocyte Donation CLICK HERE AND VISIT THE DEDICATED PAGE
Counseling
Any couple undergoing fertility treatment should be offered counselling, for several reasons that might include emotional support during often stressful treatment and coping with failure.
Another aspect of counselling is the future relationship with the assisted reproduction child and answering their questions. This is particularly relevant for treaments involving donated gamets.
Recurrent Miscarriage and Repeated IVF Failure
Recurrent miscarriage in the first trimester can have many different causes, including chromosomal disorders of the embryo itself, undiscovered genetic abnormalities in the parents, and infections of the cervix and vagina, especially Chlamydia, which may reduce fertility and cause loss of pregnancy. More rarely, uterine abnormalities and systemic illnesses may contribute to miscarriage.
Women who experience recurrent miscarriage or repeated IVF failure often suffer from immunological or haematological disorders that affect early embryo implantation, because the immune system rejects the embryo; thyroiditis and lupus erytomatosus are common causes of immunological disorders. Also, abnormalities of the clotting system negatively affect the development and functioning of the early placenta.
Laboratory investigations are able to pick up irregularities that benefit from pharmaceutical therapy. The most common therapies involve high-dose vitamins, heparin and cortisone. Sometimes additional treatment with immunoglobulins is necessary to help reduce the immunological reaction and thus the rejection of the early embryo.
Success Rates
Achieving a pregnancy is influenced by multiple factors that include maternal age, individual problems and pathologies, as well as the assisted reproductive therapy chosen. For women aged 20-35 years undergoing IVF and blastocyst transfer achieves a pregnancy rate of over 58%.
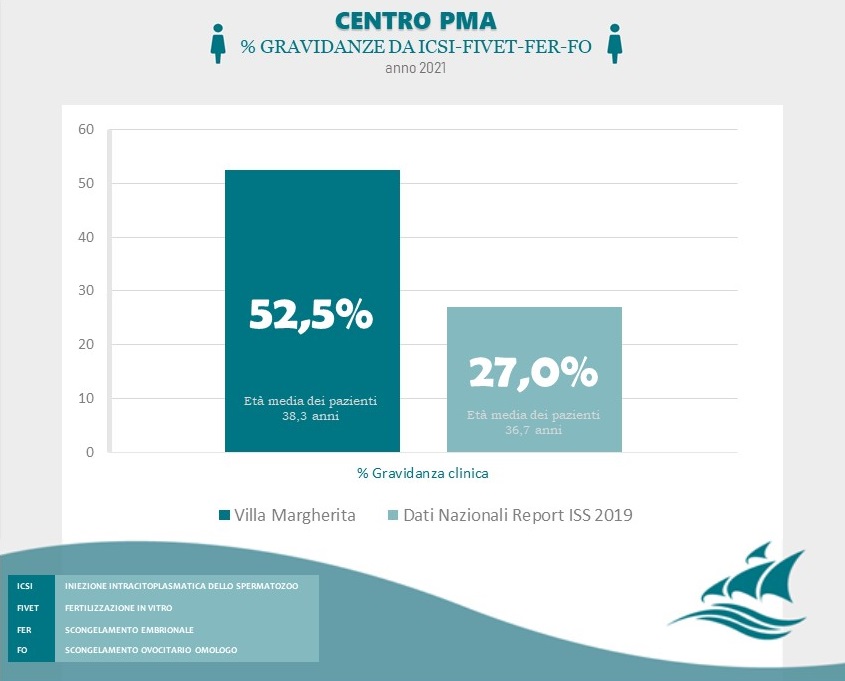
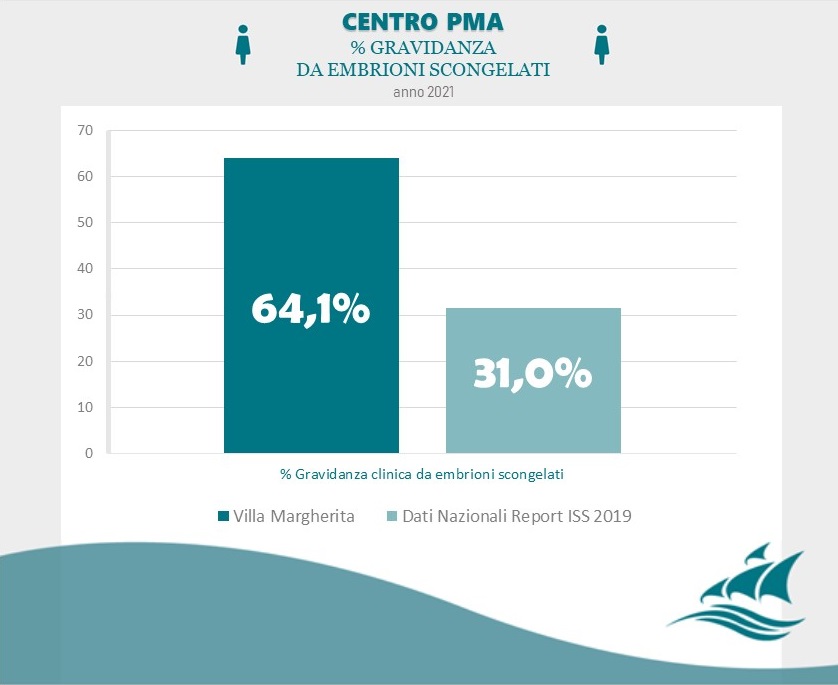
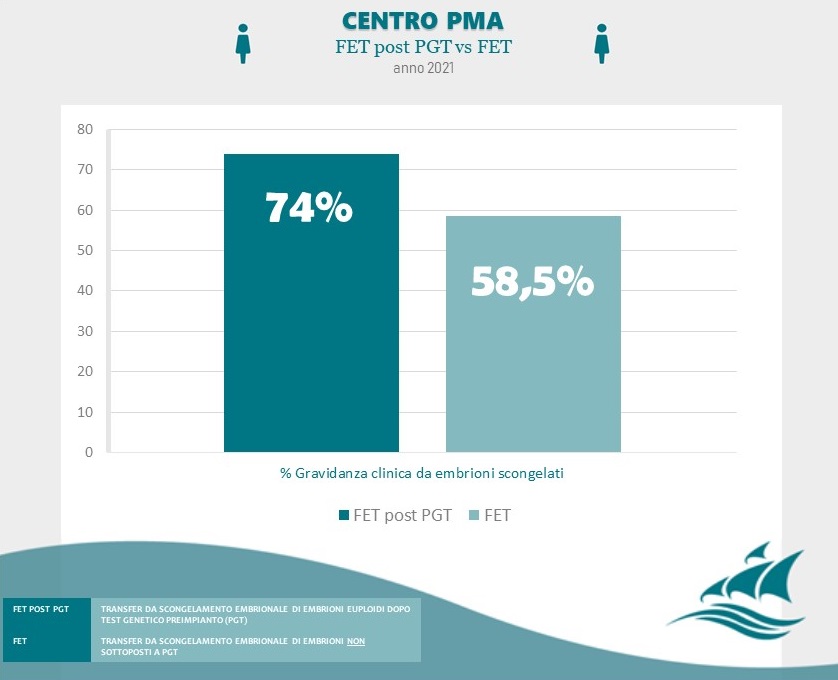
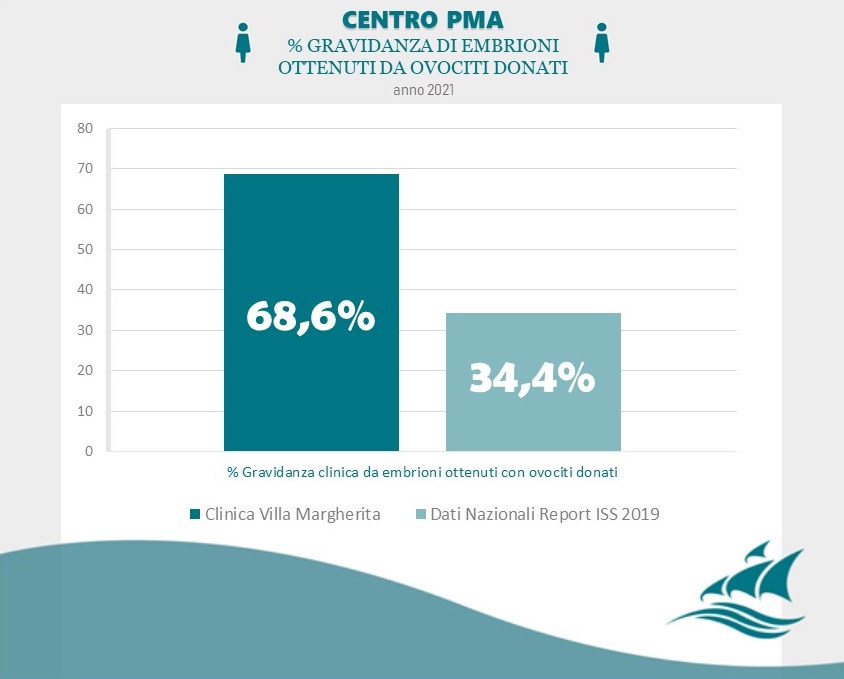
Data Source: Clinica Villa Margherita – Roma

